Pressure injury
The highest rate of pressure sores are seen in elderly patients with cardiovascular disease (41%) , neurological disease (27%), and orthopedic injury (15%).(Grabband Smith’s Plastic Surgery p 1084, 1997)

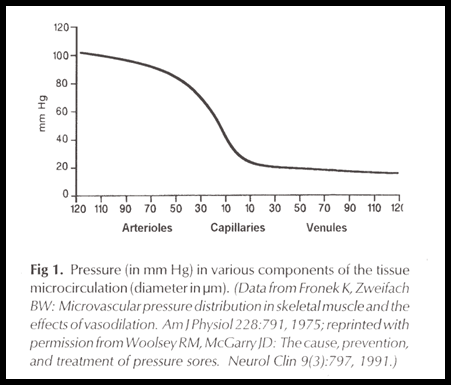
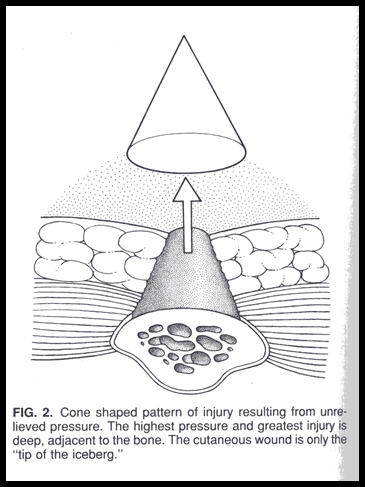
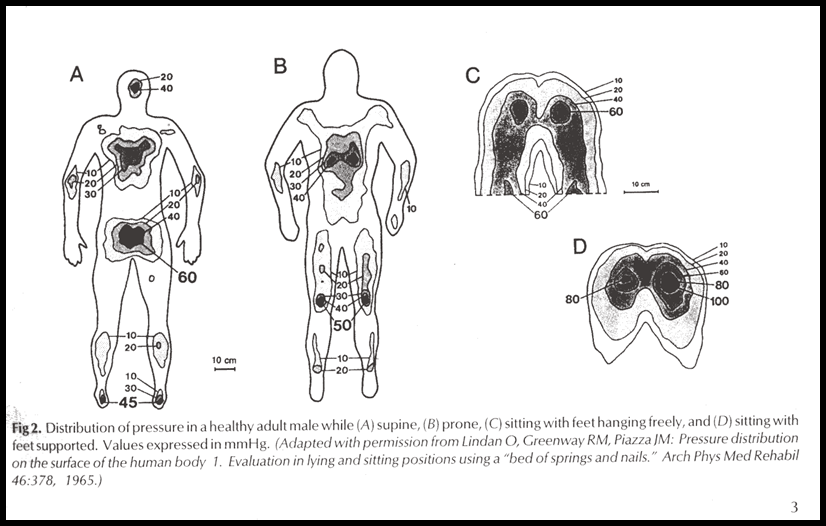
 Soft tissue issqueezed between two hard surfaces- a bed or chair on the outside of the body and a bone on the inside - creating atissue pressure thatexceeds the vascular perfusion pressure.
Soft tissue issqueezed between two hard surfaces- a bed or chair on the outside of the body and a bone on the inside - creating atissue pressure thatexceeds the vascular perfusion pressure.
* Muscle is more sensitive to pressure than skin, probably because of the higher metabolic
requirements of muscle.
* Muscle begins tonecrose after 4 hours of ischemia, whereas skin can withstand approximately 12
hours.



* The elder
* The neurological disease
the restricted mobility
the loss of sensation
fecal and urinaryincontinenece
* The hospitalization
predisposing disease
nutrition status
infection

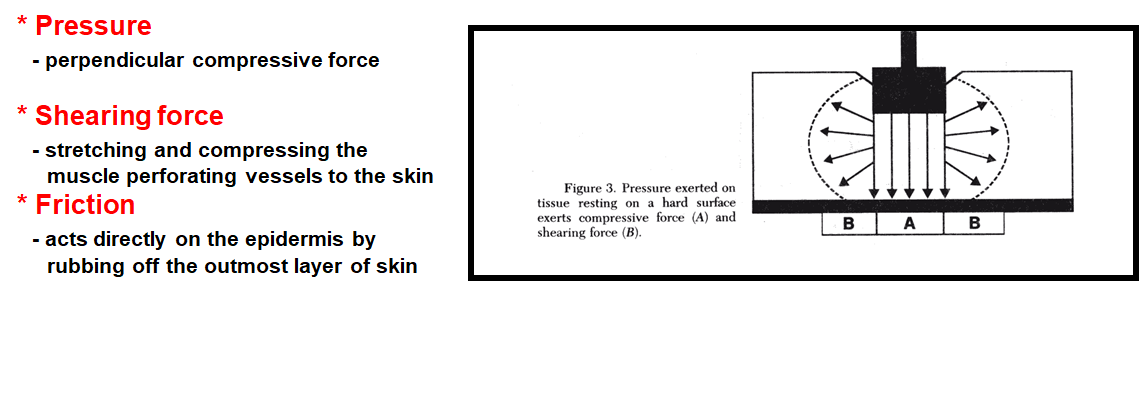
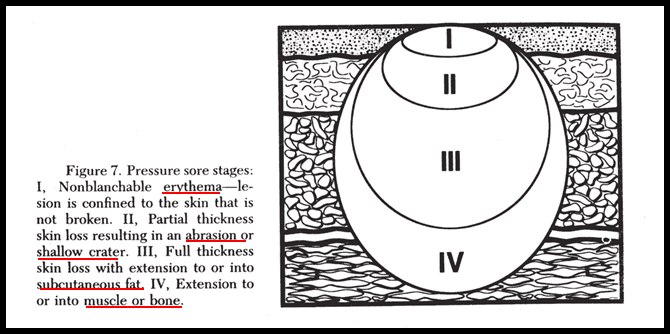
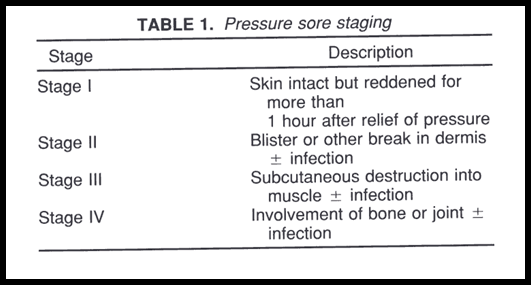
* Stage 1 and 2 pressure sores are typically caused byfriction or shear components.
* Stage 3 and 4 pressure sores arepressure-time components


* Relief of pressure
* Control of infection
* Nutrition
* Control of spasticity

*Seated patientsmust lift themselves from their chairs for at least5 minutes every 30 minutes, and recumbent patientsmust be repositioned at least every 2 hours.
* Pressure-reductive devices, composing of high-density foam, gels, water , or air-filled beds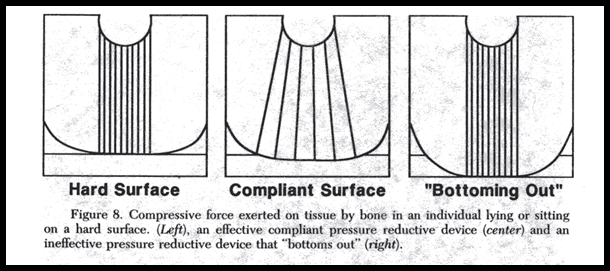

* Debridement of dead tissue
* Keep surrounding skin clean and dry
* Appropriate dressing
* Topical and systemic antibiotics

* Serum albumin > 2.0gm/dl
* Daily protein : 1.5-3.0gm/kg
* Daily caloric intake: 25-35cal/kg
*VitA&C; Zinc;Ca; Fe; Cu
* Low residual diet

* Prevent progressive osteomyelitis and sepsis
* Reduce protein loss through the wound
* Improve quality of life
* Lower hospitalized costs
* Improve patient hygiene and appearance
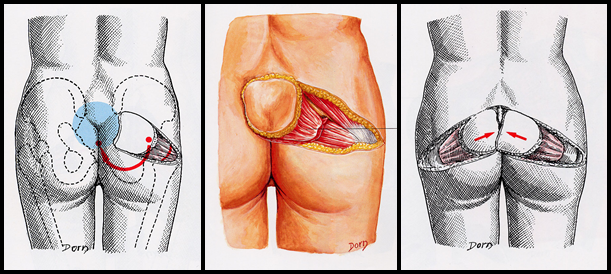
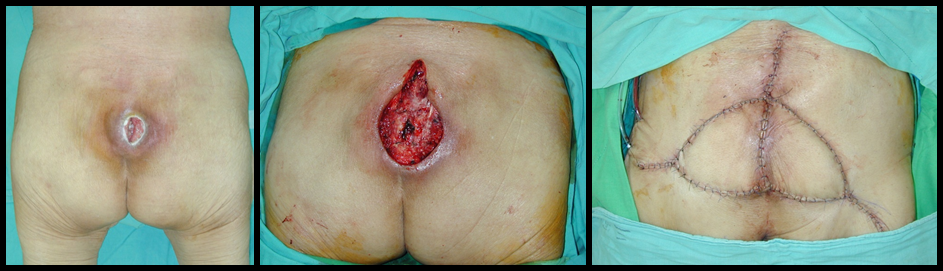

split inferior glutealmaximus myocutaneous flap




* Hematoma
* Infection
* Wound dehiscence
* Inadequate debridement
*Recurrence rate: 15-48%